The following points highlight the five major disorders of Thyroid Function. The disorders are: 1. Adult Hypothyroidism 2. Infantile Hypothyroidism 3. Physiological Disorders 4. Hyperthyroidism and Thyrotoxicosis 5. Other Common Disorders of Thyroid Function.
Disorder # 1. Adult Hypothyroidism:
In adults, the onset of hypothyroidism is usually so insidious that the typical manifestations may take months or years to appear. However, the common features include easy fatigability, coldness, weight gain, constipation, muscle cramping, rough and dry skin, puffy face-and hands, hoarse and husky voice, slow reflexes, numbness and tingling of fingers, extreme mental lethargy.
Many of these symptoms may occur in acute hypothyroidism leading to a situation commonly termed as myxedema (puffy appearance).
Disorder # 2. Infantile Hypothyroidism:
Severe hypothyroidism is seldom apparent at birth. The age at which symptoms appear depends on the degree of impairment of thyroid function. Severe hypothyroidism in infancy is termed cretinism. Its symptoms during the first few months include feeding problems, failure to thrive, constipation, a hoarse cry and somnolence.
ADVERTISEMENTS:
In succeeding months, protuberance of abdomen, dry skin, poor growth of hair and nails take place. Retardation of mental and physical development is manifested by delay in reaching the normal milestones of development, such as holding up the head, sitting, walking and talking.
Hypothyroidism in children is characterised by retarded growth and evidence of mental retardation. In the adolescent, precocious puberty may occur, and there may be enlargement of sella turcica in addition to short stature.
Disorder # 3. Physiological Disorders:
Thyroid hormone deficiency affects every tissue in the body. Pathologically the most characteristic findings are reflected in the following symptoms:
(1) Cardiovascular system:
ADVERTISEMENTS:
Hypothyroidism is characterised by impaired muscular contraction, bradycardia and decreased cardiac output. Cardiac enlargement may occur, due in part to interstitial edema, nonspecific myofibrillary swelling and left ventricular dilation but often due to pericardial effusion.
(2) Respiratory system:
In the adult, hypothyroidism is marked by shallow, slow respiration and impaired ventilatory responses to hypoxia.
(3) Alimentary system:
ADVERTISEMENTS:
Peristaltic activity is decreased, resulting in chronic constipation and occasionally severe fecal impaction or ileus. Intestinal absorption for many substances may be decreased. The colon may be greatly distended and the fluid volume in peritoneal cavity is usually increased. The liver and pancreas remain normal.
Nervous system:
Thyroid hormone is essential for the developing of central nervous system. So failure in thyroid hormone synthesis may cause fatigue, lethargy, depression or agitation. The intellectual functions including speech are slowed. Loss of imitativeness, slow wittedness and memory defects are common in hypothyroidism.
Muscular system:
In hypothyroidism, decreased muscle contraction and relaxation cause the slowness of movement and delayed tender jerk. Muscle mass may be slightly increased and the muscle tend to be firm. Severe muscle cramp, paresthesias and muscle weakness are very common.
Renal system:
Renal function is impaired, with decreased glomerular filtration rate and impaired ability to excrete a water load.
Skeletal system:
Thyroid hormone is essential for normal growth and maturation of the skeleton. Growth failure in cretinism is due both to impaired protein synthesis and to the reduction in IGF-I level.
ADVERTISEMENTS:
Anemia:
Anemia in hypothyroidism is caused at least by four mechanisms:
(i) Impaired haemoglobin synthesis,
(ii) iron deficiency from increased iron loss with menorrhagia and impaired iron absorption through intestine,
(iii) Impaired folate absorption
(iv) Pernicious anemia, with vitamin B12 deficient megaloblastic anemia.
Disorder # 4. Hyperthyroidism and Thyrotoxicosis:
Over activity of the thyroid gland or overproduction of thyroid hormone is referred to as hyperthyroidism. Thyrotoxicosis is the clinical syndrome that results when tissues are exposed to high level of circulating thyroid hormones. Thyrotoxicosis results primarily due to hyperthyroidism.
The other forms of thyrotoxicosis are discussed below in brief:
1. Graves’ disease (Diffuse toxic goiter):
Graves’ disease is an autoimmune disease which is the most common form of thyrotoxicosis. It may occur at any age and is more common in females than in males.
Pathogenesis and Physiological disorders:
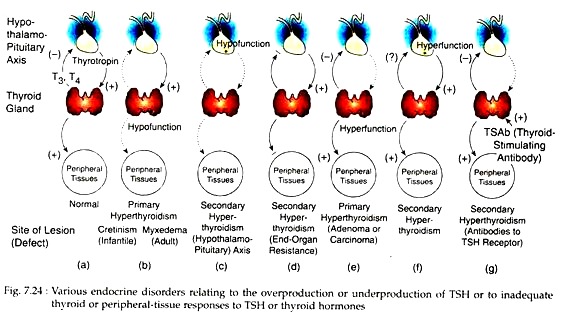
In Graves’ disease, auto-immunisation against thyroid components produces antibodies (antibody against TSH receptor or TSH-R Ab). It may bind to TSH receptors on thyroid follicle membrane and thus stimulating the action of TSH on thyroid.
Its prolonged action produces an overactive enlarged thyroid (Thyrotoxic goiter) and over-secretion of thyroid hormones (hyperthyroidism). In addition, cytokines released from sensitized lymphocytes cause thyroid-phthalmopathy. Unlike TSH, the action of TSH-R Ab is not inhibited by any feedback of thyroid hormones.
Hyperthyroidism increases blood PBI, tissue O2 coefficient, BMR, body temperature, sweating, heat sensitivity, blood pressure and heart rate, blood sugar etc. It also causes weight loss, negative N-balance, palpitation, dyspnea on exertion, tremor, nervousness, easy fatigability. Thyroid-ophthalmopathy causes swelling in orbital muscles, pro-ptosis of the globes, diplopia as well as redness, congestion and conjunctival and peri-orbital edema, limitation of upward and lateral eye movement and reduced visual activity at last stage.
2. Plummer’s disease (Toxic adenoma):
In Plummer’s disease, small lesions first slowly increase in size and gradually suppress the other lobe of the gland. As a result, T3 and T4 are over-secreted even under low TSH, resulting in hyperthyroidism. Toxic adenomas are always follicular adenomas and almost never malignant. Symptoms include weight loss, weakness, shortness of breath, palpitation, tachycardia, heat intolerance; ophthalmopathy is never noted.
3. Toxic Multi-nodular Goiter:
A suppressed TSH level and striking elevation in serum T3 levels with less striking elevation of serum T4 in association with multiple nodules, or multi-nodular goiter may occur in older patients with hyperthyroidism. Ophthalmopathy is rare in such cases, but tachycardia, heart failure or arrhythmia, sometimes weight loss, nervousness, weakness, tremors and sweating are common.
Disorder # 5. Other Common Disorders of Thyroid Function:
1. Thyroid hormone resistance syndrome:
In generalized resistance to thyroid hormone (GRTH), all of the body tissues are variably resistant to thyroid hormone. This abnormal condition is associated with high levels of thyroid hormones with normal TSH. The symptoms include stippled epiphyses goiter.
Molecular studies have revealed point mutations in the human thyroid receptor beta gene (hTR-B). It produces a defective thyroid hormone receptor which fails to bind T3 and is the main cause of GRTH.
The selective pituitary resistance to thyroid hormones (PRTH) is associated with mild hyperthyroidism, goiter, elevated serum T4 and T3 and normal or elevated serum TSH. In this syndrome, a failure of T3 to inhibit pituitary TSH secretion results in inappropriate TSH secretion and TSH-induced hyperthyroidism.
2. Nontoxic goiter:
Nontoxic goiter generally represents enlargement of the thyroid gland from TSH stimulation, which in turn results from inadequate thyroid hormone synthesis.
Different causes of such goiter are:
(i) Iodine deficiency.
(ii) Intake of goitrogen with diet.
(iii) Hashimoto’s thyroiditis.
(iv) Sub-acute thyroiditis.
(v) Inherited defect in thyroidal enzymes required for T3 and T4 biosynthesis, which lead to inadequate hormone synthesis.
(vi) Inherited defect in T4 receptors in follicle membrane.
(vii) Thyroid neoplasia, benign or malignant.
In all cases of nontoxic goiter thyroid enlargement, either diffused or multi-nodular is present. The gland may be firm but is often extremely soft. There may be symptoms of mild hypothyroidism, but most of these patients are euthyroid.
3. Thyroiditis:
In sub-acute thyroiditis or granulomatous thyroiditis, an acute inflammatory disorder of the thyroid gland is noted. It is due to infections caused by a number of viruses including mumps virus, coxsackievirus and adenoviruses.
Pathological examination reveals moderate thyroid enlargement and a mild inflammatory reaction involving the capsule. Initially, T3 and T4 are elevated, whereas serum TSH is extremely low but latter, as the disease progresses, T3 and T4 drop, TSH is high and symptoms of hypothyroidism are noted.
Chronic thyroiditis (Hashimoto’s thyroiditis, lymphocytic thyroiditis) is the major cause of goiter in children and young adults and is probably the major cause of idopathic myxedema which represents an end stage of Hashmoto’s thyroiditis, with total destruction of the gland.
It is thought to be an immunologic disorder in which sensitized lymphocytes produce three important thyroid autoantibodies viz. thyroglobulin antibody (Tg Ab), thyroid peroxidase antibody (TPO Ab) and TSH receptor blocking antibody (TSH-R Ab).
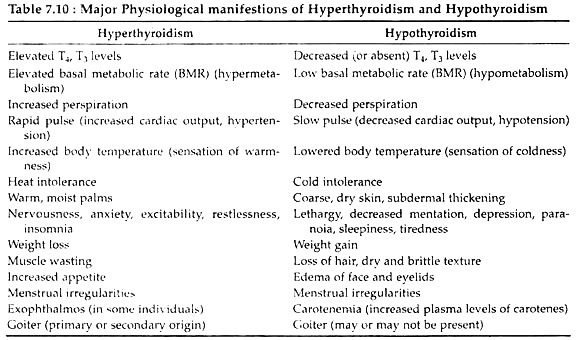
In Hashimoto’s thyroiditis, destruction of the gland results in a fall in serum T3 and T4 and a rise in TSH. Initially TSH may cause adequate hormone synthesis by development of thyroid enlargement or goiter, but often the gland fails and hypothyroidism with or without goiter ensues. A summary of the general etiology and manifestations of hypothyroidism and hyperthyroidism is provided in table 7.10 and Fig. 7.24.