The following points highlight the two main disorders in function of Adeno-Hypophyseal hormones anterior pituitary. The disorders are: 1. Hypopituitarism 2. Hyperpituitarism.
Disorder # 1. Hypopituitarism:
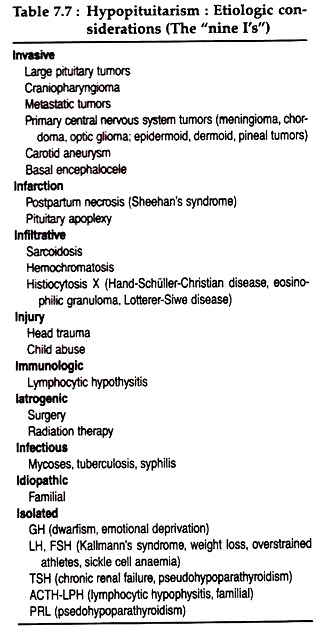
Hypopituitarism is caused either by destruction of the anterior pituitary gland or secondary phenomenon resulting from deficiency of hypothalamic stimulatory (or inhibitory) factors acting on the pituitary. However, the overall etiologic considerations in hypopituitarism are diverse as shown in table (Table 7.7). A brief description of isolated (mono-tropic) deficiencies at the anterior pituitary hormones is given.
(1) GH-deficiency:
ADVERTISEMENTS:
Congenital GH deficiency present with normal birth length show decreased growth rate soon after birth. Patients with classic GH-deficiency have short stature, obesity with immature facial appearance, immature high-pitched voice, and some delay in skeletal maturation.
Intelligence is normal in GH deficiency unless repeated or severe hypoglycemia has compromised brain development. Optic hypoplasia with visual defects is also associated with GH deficiency.
Acquired GH deficiency may result from craniopharyngiomas, germinomas, gliomas etc. Such patients, chiefly boys show constitutional delay in growth and adolescence may have transient GH deficiency by testing before the actual onset of puberty.
Children with psychosocial dwarfism present with poor growth, potbellied immature appearance, and bizarre eating and drinking habits. These children often reveal GH deficiency at first which quickly return to normal, when the patients are removed from their homes.
ADVERTISEMENTS:
(2) ACTH deficiency:
Mono-tropic ACTH deficiency is rare and is manifested by the signs and symptoms of adrenocortical deficiency. This defect may be due to primary failure of the corticotrophs to release ACTH and its related peptide hormones or may be secondary to impaired secretion of CRH by the hypothalamus
(3) TSH-deficiency:
Mono-tropic TSH deficiency is rare and is caused by a reduction in hypothalamic TRH secretion. Some patients with chonic renal failure appear to have impaired TSH secretion.
ADVERTISEMENTS:
(4) Gonadotropin deficiency:
An isolated defect in GnRH secretion is found in Kallman’s syndrome, an X-linked dominant disorder. In other sporadic cases, where anterior pituitary function is otherwise intact, young men with isolated hypo-gonadotropic hypogonadism develop a eunuchoid appearance, since testosterone deficiency results in failure of epiphysial closure.
In women, a state of hypo-gonadotropic hypogonadism is manifested by amenorrhea often accompanies weight loss, emotional or physical stress. Isolated gonadotropin deficiency may also be seen in the poly-glandular autoimmune syndrome. Other chronic illness like poorly controlled diabetes and malnutrition may result in gonadotropin deficiency.
(5) Prolactin deficiency:
Prolactin (PRL) deficiency leads to failure of postpartum lactation. Isolated PRL deficiency has been reported after lymphocytic hypophysitis and in patients with pseudohypoparathyroidism.
Disorder # 2. Hyperpituitarism:
Hyper-secretion of pituitary hormones may result from neoplasia (pituitary tumors), or from hypertrophy and hyperplasia resulting from enhanced hypothalamic stimulation of the pituitary. Hyper-secretion of PRL or α-MSH could result, plausibly from loss of a tonic hypothalamic inhibitory input to the pituitary. Micro-adenomas may be responsible for the excess secretion of a particular pituitary hormone.
Prolactinomas are the most common type, accounting for about 60% of primary pituitary tumors. GH hyper-secretion occurs in about 20% and ACTH excess in 10%. Hyper-secretion of TSH, gonadotropins, or alpha subunits is unusual. Nonfunctional tumors currently represent only 10% of all pituitary adenomas.
ADVERTISEMENTS:
Over-secretion of some pituitary hormones and their physiological consequences are described below:
(1) Prolactin excess:
PRL hyper secretion is the most common endocrine abnormality due to hypothalamic-pituitary disorders, and PRL is the hormone most commonly secreted in excess by pituitary adenomas. In the latter case, pituitary adenomas arise most commonly from the lateral wings of the anterior pituitary, but with progression they fill sella turcica and compress the anterior and posterior pituitary lobes.
In women, excess secretion of PRL causes galactorrhea, amenorrhea, oligomenorrhea with anovulation or infertility. Increased PRL inhibits both the normal pulsatile secretion of LH and FSH and the mid-cycle LH surge, resulting in anovulation.
The positive feedback effect of estrogen on gonadotropin secretion is also inhibited. Other symptoms include weight gain, fluid retention and irritability. Hirsutism may also occur, accompanied by elevated plasma levels of dehydroepiandrosterone sulfate. In men, PRL excess may cause occasional galactorrhea, decreased libido, visual impairement and impotency.
(2) GH excess:
Over secretion of growth hormone causes the classic clinical syndromes of acromegaly and gigantism. In adult GH excess leads to acromegaly, the syndrome characterised by local overgrowth of bone. Linear growth does not occur, because of prior fusion of the epiphyses of long bones.
In childhood and adolescence, the onset of chronic GH excess leads to gigantism. Excessive pituitary GH secretion could be secondary to abnormal hypothalamic function, but in most cases, it is a primary pituitary disorder. Pituitary adenomas are present in virtually all patients; and hyperplasia alone is rare.
Most of the deletorious effects of chronic GH hyper secretion are caused by its stimulation of excessive amounts of IGF-I. The growth promoting effects of IGF-I lead to the characteristic proliferation of bone, cartilage and soft tissues and increase in size of other organs to produce classic manifestations of acromegaly.
However, the insulin resistance and carbohydrate intolerance seen in acromegaly appear to be direct effect of GH and not due to IGF-I excess.
Early manifestation of acromegaly (or late gigantism) includes soft tissue proliferation with enlargement of hands and feet which is accompanied by increased sweating, heat intolerance, oiliness of the skin, fatigue and weight gain.
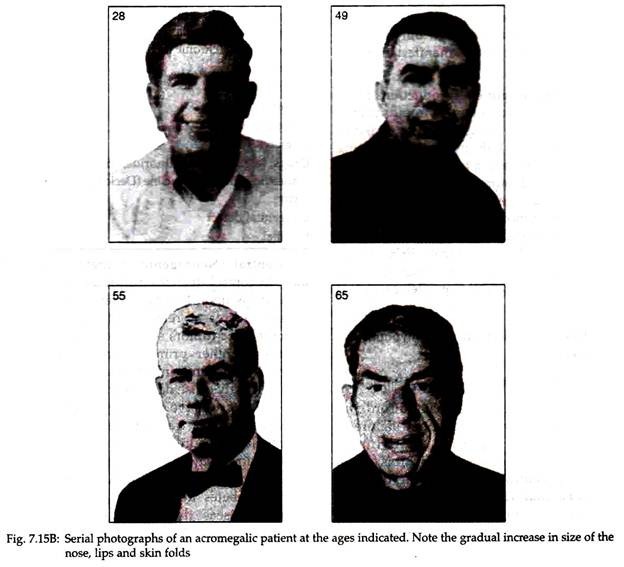
Bone and cartilage changes affect chiefly the face and skull with thickening of calvarium, increased frontal sinuses leading to prominence of the supraorbital ridges, enlargement of the nose; downward and forward growth of the mandible leading to prognathism and widely spaced teeth (Fig. 7.15B). The hands and feet are large, thickened, with blunt spade-like fingers (Fig. 7.15A) and toes.
Other endocrine and metabolic disorders are common which include GH- induced insulin resistance, hypogonadism, hyperprolactinemia etc. In men, low plasma testosterone levels may be due to GH suppression of sex-hormone-binding globulin (SHBG) levels. In persistent acromegaly, death may result from cardiovascular and cerebrovascular atherosclerosis and respiratory diseases.
(3) ACTH-over secretion:
Pituitary ACTH hyper secretion (Cushing’s disease) is the most important cause of spontaneous hypercortisolism of Cushing’s syndrome.
The endocrine disorders in Cushing’s disease include:
(1) Hyper secretion of ACTH with bilateral adrenocortical hyperplasia and hypercortisolism.
(2) Absent of circadian periodicity of ACTH and Cortisol secretion.
(3) Absent responsiveness of ACTH and Cortisol to stress (hypoglycemia or surgery).
(4) Abnormal negative feedback of ACTH secretion by glucocorticoids.
(5) Subnormal responsiveness of GFI, TSH and gonadotropins to stimulation. In fact, ACTH hyper secretion arises from a spontaneously developing pituitary adenoma and the resulting hypercortisolism suppresses the normal hypothalamic pituitary axis and CRH release and thereby abolishes the hypothalamic control of circadian release of ACTH and Cortisol.
ACTH over secretion also causes reduced sugar tolerance, hyperglycemia, glucosuria, negative N-balance, high urinary NPN, high serum levels of free fatty acids etc.
(4) TSH over secretion:
Pituitary TSH hyper secretion may result form pituitary adenomas or may not be associated with pituitary tumors. TSH dynamic is variable, TRH administration rarely stimulates TSH secretion from pituitary tumors, nor do dopamine suppresses TSH as it does in the TSH hyper secretion of primary hypothyroidism. TSH overproduction from pituitary adenomas does not show manifestations of Grave’s disease.
(5) Gonadotropin-overproduction:
Pituitary secretion of excess gonadotropins primarily results from adenomas. The majority hyper secretes only FSH, but tumors secreting both LH and FSH and a tumor secreting only LH have been demonstrated.
GnRH may or may not stimulate gonadotropin release from the pituitary tumors; testosterone levels may be low or elevated; in either case, the individuals are impotent or infertile. FSH and LH secretory dynamics are abnormal; in addition, LH and FSH secretion is often provoked by TRH.