In this article we will discuss about:- 1. Meaning of Thyroid Gland 2. Development of Thyroid Gland 3. Location 4. Anatomy 5. Histology and Cytology.
Meaning of Thyroid Gland:
Thyroid gland is the largest organ (weighing about 15-25 gm. in adult human), specialised for endocrine function in human body. This gland is capable of accumulating iodide in great excess and combining it into an organic compound thyroxine, the main hormone of thyroid.
This hormone and its precursors are virtually the only iodine compounds in living organisms. The mammalian thyroid also secretes the calcium-lowering hormone calcitonin. Dysfunction and anatomic abnormalities of the thyroid are among the most common diseases of the endocrine glands.
Development of Thyroid Gland:
The thyroid gland is an embryonic derivative of the alimentary tract. A median, unpaired sac-like evagination first appears from the floor of the embryonic pharynx. The distal end of this outgrowth gradually expands and becomes bilobed and the stalked attachment narrows to form the thyroglossal duct.
ADVERTISEMENTS:
The duct usually atrophies and two lobes become solid masses of tissue and remain connected to each other by a narrow isthmus of tissue.
Location of Thyroid Gland:
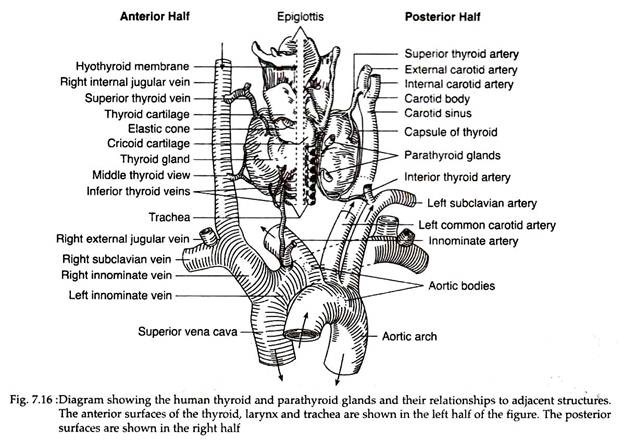
The human thyroid consisting of two lobes, each on either side of the trachea at a position just below the cricoid cartilage. The isthmus that connects two lobes extend over the anterior surface of the trachea. A pyramidal lobe near the isthmus of the thyroid may persist as a remnant of the thyroglossal stalk (Fig. 7.16).
Anatomy of Thyroid Gland:
Each lobe of human thyroid in pear-shaped and measures about 2.5-4 cm in length, 1.5-2 cm in width and 1-1.5 cm in thickness. The weight of this labile organ varies with age, reproductive status and diet. However, the normal thyroid of adult weighs 15-25 gm.
ADVERTISEMENTS:
The gland is encapsulated by two layers of connective tissues; the outer layer is continuous with the cervical fascia and is loosely connected to the inner capsule that adheres intimately to the surface of the gland.
Post-ganglionic sympathetic fibres from the superior and inferior cervical ganglia and vegal fibres from the superior and inferior laryngeal nerves enter the gland. The gland has a rich vascular supply. The superior and inferior thyroid arteries arise, respectively, from the external carotid and subclavian arteries. The thyroid ima artery arises from the brachiocephalic artery, at the aortic arch.
An important anatomical consideration includes two pairs of parathyroid glands that usually lie behind the upper and middle thyroid lobes (Fig. 7.16).
Histology and Cytology of Thyroid Gland:
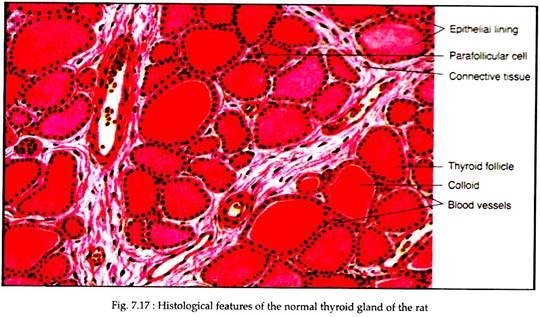
The thyroid gland is composed of an aggregation of spherical to ovate cyst like follicles of variable size. The thyroid in normal rat contains about 100,000 follicles; the larger follicles generally located near the periphery and the smaller ones in the centre.
ADVERTISEMENTS:
The inter-follicular spaces are occupied by highly vascularized network of connective tissue with few lymphocytes and histocytes. Each follicle is lined by a secretory epithelium composed of single layer of cuboidal or low columnar cells.
Surrounded by the epithelium is a closed cavity in each follicle that contains a homogeneous, gelatinous amber-coloured material. This material is called as ‘colloid’ that gives to the gland its most distinguishing histologic peculiarity (Fig. 7.17).
The follicle cells synthesise thyroglobulin, which is extruded into the lumen of the follicle and remains stored as colloid. Its density varies in different glands and in different follicles of the same gland.
When the thyroid is inactive, there is a tendency for colloid to accumulate and for the epithelium to become low cuboidal or squamous. The cells become columnar and plicated, and the colloid stores are depleted when the gland is overactive or stimulated by TSH. There are however, many exceptions, so histological examination alone cannot establish the functional state of the gland.
In the inter-follicular space as well as in the basal region of the follicles, are few ovoid cells with granular cytoplasm and irregularly-shaped nucleus. These are para-follicular cell or C cells (clear cells) of neural crest origin and secreting calcitonin.
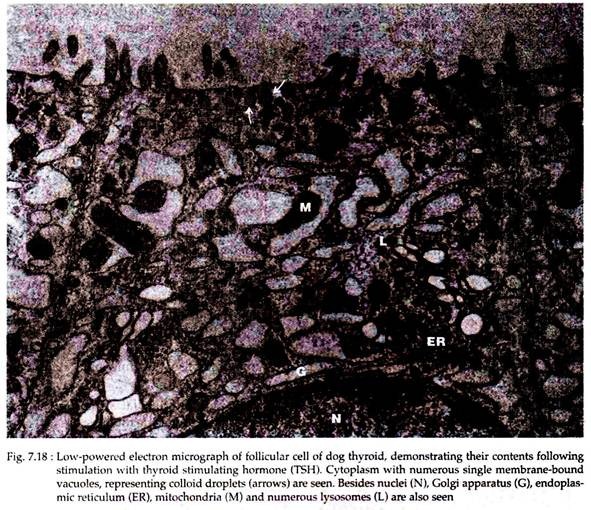
Under electron microscope (EM), the cytological features of thyroid follicle cells appear to be similar with many other secretory cells. The cells have extensive endoplasmic reticulum (ER) with dilated cisternae and laden with microsomes. An extensive Golgi apparatus (G) occurs near the apical part of the cell; mitochondria (M) and lysosomes (L) remain scattered throughout the cytoplasm.
The thyroid cytoplasm, in addition to these usual features contains a larger than usual variety of granules of different sizes and densities. The apical surface of the cells have small thin projections or microvilli (MV) which are increased in number if the gland is stimulated by TSH injection (Fig. 7.18).
Some of the granules may also be present within the microvilli. Release of entire secretion-laden cells (holocrine mode of release) is sometimes found following EM observation.