Here is a compilation of notes on hormones. After reading these notes you will learn about: 1. Meaning of Hormones 2. Characteristics of Hormones 3. Classification 4. Synthesis 5. Transport and Metabolism 6. Patterns of Secretion 7. Control of Secretion 8. General Functions 9. General Mechanisms.
Contents:
- Notes on the Meaning of Hormones
- Notes on the Characteristics of Hormones
- Notes on the Classification of Hormones
- Notes on the Synthesis of Hormones
- Notes on the Transport and Metabolism of Hormones
- Notes on the Patterns of Hormone Secretion
- Notes on the Control of Hormone Secretion
- Notes on the General Functions of Hormones
- Notes on the General Mechanisms of Hormones
Note # 1. Meaning of Hormones:
Hormones are any substances released by a cell or gland which act through receptors on another cell near or far regardless of the singularity or ubiquity of the source and regardless of the means of conveyance – blood stream, axoplasmic flow, or immediate intercellular space.
ADVERTISEMENTS:
Example:
Insulin, estrogen, gastrin etc.
Note # 2. Characteristics of Hormones:
Following criteria are considered while characterizing hormones in general.
ADVERTISEMENTS:
1. Chemical nature of hormones:
Chemically, hormones may be grouped into three general categories:
(a) Amines:
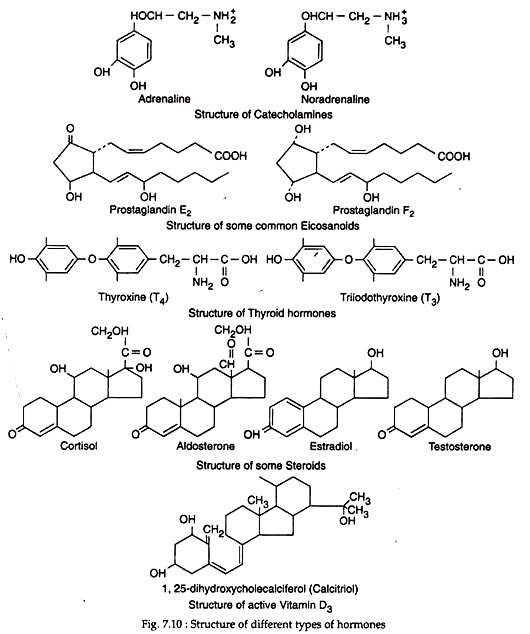
This category comprises of hormones that are derived from single amino acid. For example, thyroid hormones derived from iodinated amino acid, tyrosine, and norepinephrine, epinephrine, dopamine are derived from the amino acid tyrosine.
ADVERTISEMENTS:
(b) Proteins and peptides:
These hormones are protein in nature. The individual hormone could be referred to as peptide, polypeptide or protein in nature, depending on their specific chain length. For example, thyrotropin releasing hormone (TRH) is composed of only 3 amino acids (small peptide), while pituitary gonadotropins possess as many as 180 amino acids (large peptides).
(c) Steroid hormones:
These hormones are derivatives of cholesterol. For example, adrenal and gonadal steroids have intact steroid nucleus, while vitamin D has broken steroid nucleus. Besides the above hormones, prostaglandins, prostacyclins, leukotrienes, which are related to hormones, are derived from fatty acids.
Note # 3. Classification of Hormones:
Hormones may be classified variously. Hormones in broader sense refer a number of substances that have already been defined. Here types of hormones according to their chemical nature will be discussed. Hormones are derived from major classes of compounds that are used for general function within the body.
Thus, they are either proteins or derived proteins or amino acid analogues or lipids. When the structure of a hormone is known it is referred to as such but when their activities have been isolated but structures are not known, they are referred to as factors.
According to the chemical origin hormones may be of following types:
(1) Peptides:
ADVERTISEMENTS:
Peptide hormones are composed of amino acids, the number of which may be as few as 3 amino acids (e.g. thyrotropin releasing hormane or TRH) to as many as 180 or more (e.g. pituitary gonadotropins). However, individual hormone may be referred to as peptide (with small number of amino acids), polypeptide or protein (with single or more long chains of amino acids.) in nature depending on their specific chain length.
The amino acid chain may be linear as found in α-MSH or may be ring like as found in neuro-hypophyseal hormones (oxytocin and vasopressin). Some hormones may have more than one chain, such as insulin which has two polypeptide chains.
All peptide hormones are direct translation products of specific mRNA, but may be cleavage products of larger precursor (e.g. insulin) proteins, or modified peptides (e.g. FSH, TSH are glycoproteins).
(2) Thyroid hormone:
Thyroid gland secretes two hormones; the triiodothyronine or T3 and tetraiodothyronine or T4. These hormones are derivatives of amino acids. They are derived from the amino acid tyrosine with which an inorganic ion, (i.e., iodine) is incorporated. These hormones are indispensable for normal growth and development.
(3) Steroids:
Steroid hormones are derived from cholesterol which, in turn, is produced either by de novo synthesis or by uptake of low density lipids (LDL) through LDL receptors. Steroid hormones are produced in the adrenals, ovaries, testes, placenta and to some extent in peripheral tissues. The overall pathways in these organs are similar, though difference in the specific enzymes present in the various cells generates different final products.
(4) Vitamin D:
In animal the vitamin D3 (cholecalciferol) acts as the precursor of the active vitamin D3 or Calcitriol (or 1α, 25-di-hydroxycholecalciferol) which behaves as hormone. It acts via binding to a soluble calcitriol receptor protein belonging to the steroid T3-retinoid receptor superfamily. This hormone mainly regulates calcium and phosphate metabolism.
(5) Catechol-amines:
Catechol-amines are synthesised from the amino acid tyrosine and then stored in granules analogous to those that secrete polypeptide hormones. Two important catechol-amines are epinephrine and norepinephrine which are synthesised mainly by adrenal medulla. Dopamine is another catecholamine. Catechol-amines also act as neurotransmitter.
(6) Eicosanoids:
Eicosanoids are hormone-related substances that are derived from fatty acids. Common examples of this hormone include prostaglandins, prostacyclins and leukotriene. The arachidonic acid is the most important and abundant precursor of the various eicosanoids in humans.
Arachidonic acid in turn is formed from the essential fatty acid linoleic acid. Eicosanoids play significant roles in many physiological processes (Fig. 7.10).
Note # 4. Synthesis of Hormones:
Like all other proteins, peptide and protein hormones are synthesised in the rough endoplasmic reticulum. Their amino acid sequences are determined by specific mRNA having definite nucleotide sequences dictated by specific gene. Translation of such mRNA results in the ribosomal synthesis of a protein, usually larger than the mature hormone.
This precursor is referred to as pro-hormone or preprohormone. The pro-hormone is extended at their amino termini by a hydrophobic amino acid sequence called leader or signal peptide. Preprohormones in addition to signal peptides, also contain internal cleavage sites that yield different bioactive peptides upon enzymatic action.
With the aid of hydrophobic leader peptide, the hormone precursors move across the ER membrane to be transported to Golgi complex. The leader sequence is removed before the synthesis of polypeptide chain has ended and this permits the protein to gain its secondary structure during its transport to Golgi.
Following its arrival at Golgi the pro-hormones may be processed by proteolytic enzyme to generate mature hormones, and /or by other enzymes that add nonprotein residues such as carbohydrates in case of glycoprotein hormones (e.g., FSFI, LH).
Whatever the case, the hormone stored in vesicles will fuse the cell membrane during their release and their contents will be extruded into the extracellular perivascular space. This process is called exocytosis, which is the most common process of hormone release.
The synthesis of amine and steroid hormones are different from that of peptide hormones. Amine and steroid hormones originate from the precursor molecule tyrosine and cholesterol, respectively.
Within the cells of synthesis, these precursor molecules are subjected to the sequential action of several enzymatic catalysis resulting in the formation of various intermediate products that themselves may be hormones. In contrast to peptide hormones, thyroid hormone and steroids, once produced, can freely cross the cell membrane without having to be packed in granules and are actively exocytosed.
There are ample examples of hormones that are produced at sites other than those in which their precursor is formed. In some cases, a hormone with less activity is converted into an active form by the action of enzymes in the circulation or other tissues.
3. Delivery of hormones:
Hormones (in broader sense) may be delivered from the site of synthesis to their target organ or cell by one of several ways:
(i) Endocrine, when the hormones are released into circulation directly;
(ii) Paracrine, when the released hormones diffuse to its adjacent target cells through immediate extracellular space;
(iii) Autocrine, when following release, the hormone is feed backed on the cell of origin;
(iv) Neuroendocrine, when the hormone released by a nerve is blood borne;
(v) Neurocrine, when a neuron releases its hormone into a synaptic cleft between two adjacent cells,
(vi) Luminal, when a hormone is released into the lumen of the gut.
Note # 5. Transport and Metabolism of Hormones:
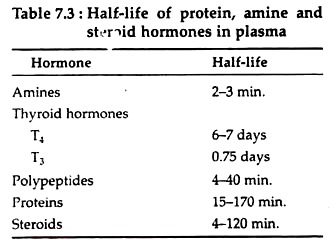
Following the release to outside from site of synthesis, hormones may circulate freely into the bloodstream or it may be bound to a carrier protein. In general, amines, peptides and protein hormones circulate in free form, whereas, steroids and thyroid hormones are bound to transport proteins (carrier proteins).
An exception to this rule is provided by insulin-like growth factors which despite being polypeptide, circulate tightly attached to specific proteins. Most common carrier proteins include thyroid hormone-binding globulin (TBG) that carry thyroid hormone, testosterone-binding globulin (TeBG) and cortisol-binding globulin (CBG) that carry testosterone and Cortisol, respectively.
Hormones, either initiate immediate target tissue responses or set in motion more long-term effects. In either cases, hormones must be continuously inactivated or the cellular response would be continuously activated. The metabolic clearance rate (MCR) of a hormone defines quantitatively its removal from plasma.
Under steady state conditions, the MCR represents the volume of plasma cleared of the hormone per unit of time. The plasma half-life of a hormone is inversely related to MCR (Table 7.3). Only a little portion of circulating hormones is removed from the circulation by most target tissues.
The bulk of hormone clearance is done by the liver and the kidneys where a number of enzymatic degradations occur that include hydrolysis, oxidation, hydroxylation, methylation, decarboxylation, sulfation and glucoronidation. In general, only a small fraction (<1%) of any hormone is excreted as such through urine or feces.
Note # 6. Patterns of Hormone Secretion:
The basal secretion of most hormones is not a continuous process but rather has a pulsatile nature. The pulsatile pattern of hormone secretion is characterised by episodes of release that can be as frequent as every 5-10 minutes; each episode is followed by a quiescent period during which plasma levels of hormone fall toward basal values.
Another discharge then occurs and the cycle repeats itself, often varying in both amplitude and frequency of the pulses. In the case of hormones subjected to negative feedback control, removal of the inhibitory feedback signal results in a marked enhancement of the amplitude and frequency of episodes of secretion.
Most prominent episodes of release may occur with a frequency of about an hour, this mode of release is called circhoral; when episodes of release occur at intervals longer than an hour but less than 24 hours, the rhythm is called ultradian; if the periodicity is of about a day, the rhythm is called circadian and if it occurs every day it is called quotidian or diurnal (e.g. ACTH).
Some hormones may have a much less periodicity. For example, the monthly pre-ovulatory discharge of gonadotropins recurs about every 30 days, a pattern of release known as circatrigintan. Thyroxine exhibits changes in plasma levels that occur over months. If the changes take place on a yearly basis, the rhythm is called circannual or seasonal.
Note # 7. Control of Hormone Secretion:
(i) Neural control:
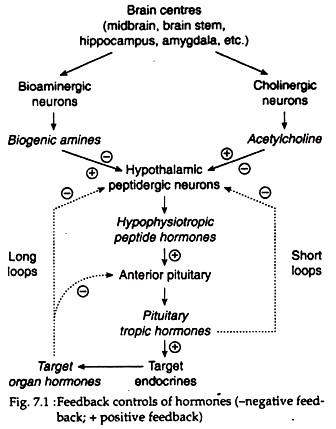
Nerve impulses control some endocrine secretions. For example, during stress and emotion, splanchnic nerve stimulates the synthesis and release of catecholamines from adrenal medulla. Nerve impulses from hypothalamic osmoreceptors evoke secretion of vasopressin from neuro-hypophyseal axon-terminals. Impulses from brain, hippocampus, amygdala and other limbic system areas may cause release of acetylcholine and biogenic amines at their axon-terminals that in turn, regulate the release of different hypo-physiotropic hormones such as GHRH, CRH, and TRH from hypothalamus.
(ii) Endocrine control:
Hormones often regulate hormone secretion from other endocrine glands. For example, secretion of adrenocortical, gonadal and thyroid hormones are stimulated respectively by corticotropin (ACTH), gonadotropins (GTH) and thyrotropin (TSH), which are as such tropic hormones of anterior pituitary that in turn are regulated by hypothalamic hypo-physiotropic hormones such as CRH, GnRH and TRH, respectively.
(iii) Feedback controls:
The secretion of a hormone may be stimulated or inhibited by the feedback effect of some other hormone or metabolites.
1. Negative feed-back control:
A high blood level of a hormone may inhibit the secretion of that hormone. It is shown by target gland hormones that inhibit the secretion of their tropic hormones. For example, high levels of Cortisol from adrenal cortex may inhibit the secretion of pituitary-corticotropin release and corticotropin-releasing hormone (CRH) from hypothalamus through long-loop feedback, all these lead to decline in Cortisol secretion itself.
High levels of tropic hormones sometimes inhibit the secretion of corresponding releasing factor from hypothalamus through short-loop feedback (Fig. 7.1). Sometimes, blood level of some ions or metabolites also shows feedback control over hormone release. For example, a rise in serum Ca2+ causes rectilinear fall in parathyroid hormone; rise in blood glucose causes a decline in glucagon secretion.
2. Positive feedback control:
Hormone- secretion may be stimulated by a positive feedback effect of another hormone or ion or metabolite. For example, sharp pre-ovulatory rise in LH secretion from anterior pituitary occurs in response to high blood level of estradiol; elevated serum calcium level causes stimulation of calcitonin release from thyroid gland.
Furthermore, some hormones may exert a negative feedback on the cells within which they are synthesised by a so-called auto-inhibition (For control of specific hormones, see different endocrine glands).
Note # 8. General Functions of Hormones:
Hormones control the activity of almost all cells in the body. However, their functions, in general, may be exerted in four broad physiological areas. These are growth and development, reproduction, maintenance of internal environment, and regulation of energy balance:
1. Growth and Development:
Many hormones exert primary and permissive roles in timing and progression of growth, both for overall body and for individual tissue. Classical examples of growth regulating hormones include GH, thyroid hormones, glucocorticoids, androgens and estrogens. The stimulatory effect of GH only on body growth is mediated by a group of peptides called insulin-like growth factors (IGFs).
Again, in absence of thyroxine, GH fails to stimulate skeletal growth, a phenomenon that appears to be regulated to a reduced ability of the tissue to respond to IGFs. Hormones also play a regulatory role in the earliest aspects of cell division and differentiation of the fertilised eggs.
2. Reproduction:
Most aspects of reproduction including growth and structural integrity of reproductive organs, production of gametes, patterns of sexual behaviour, sexual differences etc., are controlled by the interaction of hormones produced by gonads, anterior pituitary (GTH) and growth hormone, Estrogens in females and testosterone in males play fundamental roles in the development of primary and secondary sexual organs.
Ovulation in females and spermatogenesis in males are processes that are tightly controlled by the pituitary gonadotropins (LH and FSH), which act either directly on the gonads to promote follicular development (ovary) and formation of sperm (testis) or indirectly through their stimulatory effects on estrogen and testosterone secretion.
3. Maintenance of Internal Environment:
Homeostasis in internal environment is maintained through the control of extracellular fluid volume and blood pressure, electrolyte composition of body fluid, regulation of plasma and tissue levels of calcium and phosphate ions, and the maintenance of bone, muscle and body stores of fats.
A number of hormones regulate these processes e.g. vasopressin, aldosterone regulate the electrolyte and water balance, thus, in turn, regulate blood pressure and extracellular fluid volume.
Plasma levels of calcium and phosphate are controlled by parathyroid hormone (PTH), 1, 25-di-hydroxy-vitamin D3 and calcitonin. The general functions of bone, muscle and adipose tissue are regulated by hormones as diverse as PTH, estrogens, androgens, GH, catechol-amines, insulin, glucagon and glucocorticoids.
4. Regulation of Energy Balance:
For an organism to survive, maintenance of energy homeostasis requires a balance between food consumption and energy expenditure. The hypothalamus plays a central role in this process by integrating a variety of afferent sensory, visual, biochemical, and hormonal signals reflecting the nutritional status of the organism.
All these signals are processed to activate efferent signals that regulate both feeding behaviour and energy expenditure. Energy expenditure in turn, is regulated via mechanisms controlling the metabolic rate, such as those influenced by the sympathetic and parasympathetic nervous systems and by insulin, glucagon and thyroid hormones.
Recent identification of the peptide leptin as a hormone produced by white adipose tissue reveals that it acts on brain (as lipostat or adipostat) to decrease food intake and increase energy expenditure. Like leptin, three other peptides – MC4-R, urocortin and bombesin receptor type-3 are known to suppress feeding behaviour.
On the other hand, two novel neuropeptides termed as orexin A and B were identified to stimulate feeding behaviour. All such factors control the energy homeostasis of an organism.
Note # 9. General Mechanisms of Hormone Action:
Higher mammals including human produce more than 100 different hormones, each of which is capable of interacting with one or more types of cell distributed in tissues throughout the body. The question is what mechanism or characteristic of a cell determines whether it will be responsive to a particular hormone.
The major factor determining the tissue response to a hormone was found to be due to some molecular components of a cell, the so-called receptors. Hormone receptors are proteins occurring in the plasma membrane, nuclear or extra- nuclear sites such as endoplasmic reticulum or cytosol that possess a hormone-binding site and a signal transducer or DNA- binding site.
Receptor provides the means by which hormones initially interact with cells.
Each receptor serves two critical functions:
1. Recognition of the hormone as an entity distinct from all of the other substances present in blood or extracellular fluid, and
2. Transformation of the binding interaction into a signal that modifies cellular metabolism and/or growth.
Each cell type of an organism does not possess receptors for all hormones, but rather only a limited number of receptor types. Some hormones stimulate a number of tissues, which implies that each of the diverse tissue possesses receptors for those hormones, for examples, insulin stimulates glucose uptake by hepatocytes, fat cells and some muscle cells, and interact with many other cell types.
When more than one tissue responds to a particular hormone at one time, it might be expected that all different physiological responses would complement the physiological process being regulated. At normal physiological levels, each hormone interacts with its own specific cellular receptor.
For example, estradiol interacts with estrogen receptors, not with other steroid receptors. Thus, hormone receptors possess a recognition function that then must be converted into the hormone’s biological functions.