In this article we will discuss about ABO and Rhesus blood group systems.
ABO Blood Group:
The ‘father of immunohaematology’, Dr. Landsteiner, first described the ABO blood group system in 1900. He observed that the serum of others agglutinated the red cells of some individuals. Detailed report of these phenomena heralded the discovery of the first human blood groups.
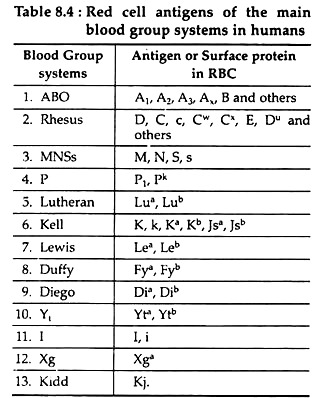
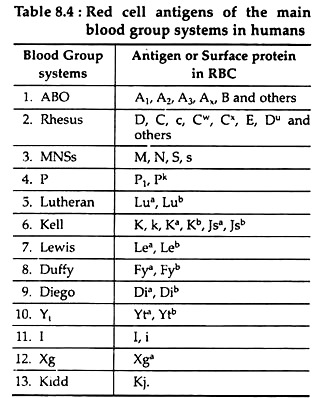
His limited experiment on laboratory colleagues, demonstrated three distinct group; his pupils Von Decastello and Sturli discovered the fourth group (AB) in 1902. Subsequent researches in this line yields a large number of blood group systems (Table 8.4). Among these systems ABO and Rhesus systems are particularly important. Transfusion from a person of one blood group into someone of another may be fatal.
Mode of Classification of Blood Groups:
People can be classified into one of several blood groups depending on the presence or absence of certain membrane substances of red blood cells, called antigens (agglutinogens). Antibodies (agglutinins) are present in the plasma, which are proteins (immunoglobulin) produced as defense mechanism when any foreign substance entered into the blood.
ADVERTISEMENTS:
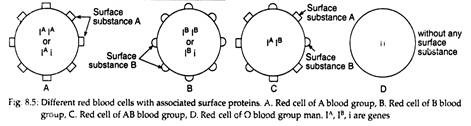
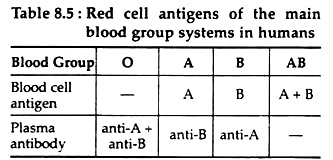
The red cells of the people of A-blood group possess A-membrane substance or A-antigen (Fig. 8.5). Similarly, red cells of B-blood group people possess B-antigen. Correspondingly, plasma of A-blood group people possesses anti-B antibodies. While plasma of B-blood group people possess anti-A antibodies (Table 8.5).
These antibodies are immunoglobulins of the IgM category. They appear soon after birth and are present throughout life. They are called iso-antibodies as distinct from immune antibodies which appear after an immune response. Production of iso-antibodies may decline and disappear in old people.
ADVERTISEMENTS:
People having red blood cells with both A and B antigens belong to group AB (Table 8.5). Their plasma is without any antibody for A and B. The people whose red blood cells do not have any membrane antigens, belongs to group O. Their plasma possesses both the antibodies for A and B -antigens. (Table 8.5).
Genetics or Inheritance of ABO Blood Group:
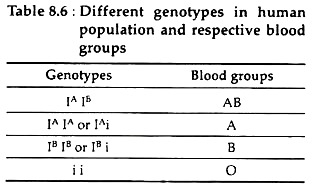
Various evidences proves that the blood properties are determined by a series of three allelic genes, IA, IB and i. IA is a gene for the production of the antigen-A on the red blood cell membrane, IB for antigen-B and i for neither antigen (Table 8.6, Fig. 8.5). The alleles of these genes act in such a way that in a heterozygous combination IAIB each allele produces its own characteristic and specific effect.
The red cells of the heterozygote contain both antigen A and antigen B (Fig. 8.5). On the other hand, IA and IB both show complete dominance over i. Therefore, heterozygous IAi and IBi produce A and B antigens respectively, while homozygous ii, lacks both antigens (Table 8.6).
Antigen Chemistry:
The ABO substances are complex oligosaccharides. These oligosaccharides that determine the specific nature of the ABO substances appear to be mostly present in glycosphingolipids.
Further Development:
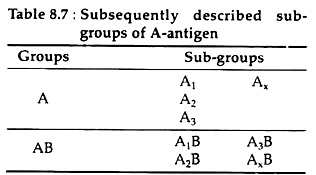
After Landsteiner’s discoveries it was noticed that the cells from some group A people react more strongly than those of others when mixed with anti-A. This led to the discovery of sub-groups of A and AB called A2 and A2B. They were first described in 1911 by Von Dungern and Hirszfeld (Table 8.7):
Significance of Blood Group in Blood Transfusion:
Only blood of same group within the ABO system is normally transfused. Incompatible transfusions may bring A (or B) antigen into contact with anti-A (or anti-B) antibodies. If this happens, the transfused cells are made to agglutinate by the antibody and they hemolysis. This transfusion reaction is normally fatal.
People of group O have red cells which possess neither A nor B-antigen and have been described as universal donors. Similarly, people of group AB have plasma containing neither anti-A or anti-B antibodies. They have been called universal recipients. These terms have fallen into disuse nowadays. Since the term universal means in all possible circumstances and takes no account of blood group systems other than ABO.
Rhesus System:
Landsteiner and Levine described the rhesus blood group system in 1940. They injected some red cells from rhesus monkeys into rabbits. Then they exposed human red cells to blood serum extracted from the rabbits. The cells from about 85% of the people whose blood was tested-agglutinated.
Therefore, it can be said that these people’s red cells must have had the same antigen as that of monkey’s red cells. This will happen, because, when rabbit’s blood was exposed to monkey’s red cell, it produced anti-monkey antibody.
If this antibody agglutinates human red cells, the above result will come out and the actual fact was that. The red cell surface substance of man which is similar to monkey’s is called the Rhesus factor (Rh-factor) or D-antigen. Now, it is known that there are many variants of D (Table 8.4).
Genes and Chemistry of Rh-factor:
Three closely linked genes appear to be involved, located on chromosome number 1, to produce rhesus factors in man. In one system of nomenclature, the products of these alleles are designated as C or c, E or e and D or d; though no product corresponding to d has yet been identified.
ADVERTISEMENTS:
The D-antigen (Rho) is the major antigen of interest. It appears to be an integral membrane protein of the red blood cell, with a molecular mass of about 30k Da. It is to be noted that Rh system is a very complex system, and neither its genetic basis nor the biochemical nature of gene products has yet been clearly elucidated.
Importance/common Functions of Rh-factors:
Generally, the people with red cells having D-antigen are called rhesus positive/ Rh+, those without D-antigen are rhesus negative or Rh–. There is no corresponding iso-antibody. However, transfusion of Rh+ cells into Rh– individual may stimulate a humoral immune response in the recipient.
The anti-D antibodies produced, causes agglutination of and haemolysis of the transferred cells, i.e. a transfusion reaction. By accounting for the rhesus and ABO groups of patients requiring blood, adverse reactions following transfusions have become very rare.
Complications arise sometimes when a Rh– woman bears a Rh+ foetus. During normal pregnancy there is no mixing of the foetal and maternal blood cells, although the two circulations run close together in the placenta. However, when the child is born, the severe contractions of the uterine wall may squeeze significant number of foetal red cells into the mother’s blood.
Some days later the mother’s immune system may produce anti-D antibody. Anti-D belongs to the IgG category of immunoglobulins. It is capable of crossing the placental membranes and entering the blood of any foetus the woman may bear in the future. If the foetus is Rh+ then the anti-D antibodies cause a transfusion reaction in foetal circulation.
The reaction is called haemolytic disease of the new born (HDNB). It can be treated successfully by giving the foetus several transfusions while it is developing inside the uterus. An alternative is to avoid the problem of HDNB by injecting a Rh– mother with anti-D antibodies immediately after she has given birth to her Rh+ child. Any of the foetal cells which may have entered her blood are thus destroyed before the trigger for the immune response.