In this article we will discuss about the Plasmodium:- 1. Introduction to Plasmodium 2. Etymology of Plasmodium 3. Habit and Habitat 4. Life Cycle.
Introduction to Plasmodium:
Plasmodium sp. require two types of hosts; an invertebrate (mosquito) and a vertebrate (reptile, bird or mammal). Technically the invertebrate host can be considered as definitive host because sexual reproduction occurs there.
Asexual reproduction takes place in the tissue of vertebrate, which thus can be called the intermediate host. However, the gametocytes actually form in the blood of the vertebrate and fertilization occurs while still in this medium in the stomach of the mosquito. For this reason, vertebrate is the definitive host.
In 1880, Charles Laveran discovered that the red blood cells of a patient suffering from malaria had the presence of some amoeba like organisms, which he termed as Plasmodium.
Laveran, then injected the blood of a malaria patient into the blood stream of a healthy person and observed that fever developed in the injected healthy person. Later, in 1889, Sir Ronald Ross in Calcutta experimentally worked out the intermediate host of this parasite and the methods of transmission of this disease.
Etymology of Plasmodium:
ADVERTISEMENTS:
Greek: plasma, something formed; edios, appearance.
Species Parasitic to Man:
Four species of malarial parasites are known to infect man. They are Plasmodium malariae (Laveran, 1881) Grassi and Feletti, 1890. Plasmodium vivax (Grassi and Feletti, 1890). Plasmodium falciparum (Welch, 1897). Plasmodium ovale.
Species Parasitic to Other Animals:
ADVERTISEMENTS:
About 60 species of Plasmodium are known to cause malaria in apes, monkey, bats, birds (sparrows, duck, domestic fowls etc.) and cold-blooded animals like lizards. Transmission of human and monkey parasites is effected by anopheline mosquitoes while that in birds is effected by culicine mosquitoes.
Antiquity of Malarial Parasites:
The high host-specificity suggests a long association between man and Plasmodium. However, it has been suggested that it existed in the primates, prior to the evolution of man. The high tolerance of malarial infection amongst the Negro races, points to Africa as the source of primitive origin.
Amongst the various malarial parasites infecting man P. malariae is regarded as the oldest and P. ovale as the most recent species. This has been further corroborated by the host’s reaction with particular species of Plasmodium.
ADVERTISEMENTS:
P. malariae has progressed from parasitism to commensalism; P. vivax has adapted itself to its host in causing benign manifestations; while P. falciparum has a poor adaptation, having unlimited power of invasiveness to host and exhibiting severe manifestations, often ending fatally. P. vivax, P. malariae, P. falciparum and P. ovale cause benign tertian, quartan, malignant tertian and ovale tertian fever, respectively.
Habit and Habitat of Plasmodium:
Plasmodium infecting man resides in its red blood corpuscles and is distributed in all the organs, through the circulating blood. This endoparasite is widely spread in the tropical and many temperate countries of the world.
Life Cycle of Malarial Parasite:
The malarial parasite completes its life cycle in two stages or cycles of development. The asexual cycle is completed in man while the sexual cycle develops in the female Anopheles mosquito.
(i) Asexual Reproduction (Human Cycle):
This stage consists of the splitting of a fully grown parasite into a number of smaller ones (merozoites). This process of development is called the cycle of schizogony (Greek: schizo, to split; gone, generation). On account of this asexual method of reproduction, man represents the intermediate or secondary host of this parasite.
(ii) Sexual Reproduction (Mosquito Cycle):
The gametocytes are first formed in the human host and if they remain in the human blood, they perish without any further change taking place. The mosquito cycle consists of the development of sexual forms.
The gametocytes are transferred from the human host to the insect host, where further development takes place. Inside the stomach of mosquito, maturation of gametocytes and fertilization occur. Further phases of development and multiplication results in the formation of sporozoites which become infective to man.
ADVERTISEMENTS:
Etymology:
Latin: vivere, to live
Life Cycle of Plasmodium:
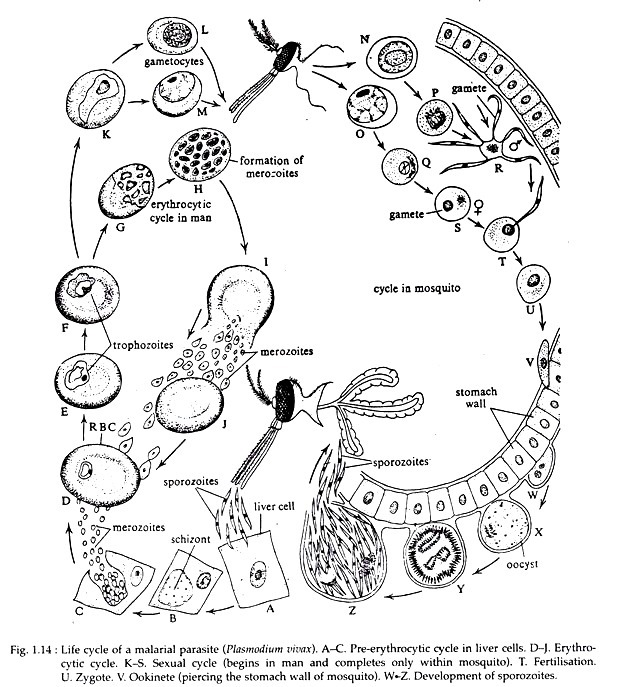
The life cycle of Plasmodium vivax (Fig. 1.14) may be divided into the following stages:
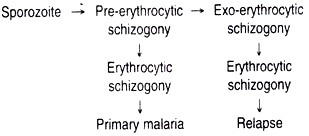
A. Pre-erythrocytic Cycle:
It begins with the inoculation of the parasite as sporozoite by the bite of the infected female. Anopheles mosquito into the blood stream of man. The blood during this sub-inoculation period of eight days is found to be non-infectious.
The sporozoites are slender and spindle shaped, measuring 15 µm in length and 1 µm in breadth. Electron microscopic study of the sporozoites of Plasmodium reveals that its external covering or pellicle consists of 3 layers and contains longitudinally arranged hollow peripheral fibrils or microtubules.
The number of microtubules in Plasmodium vivax is 11. Its anterior end bears a cup-like depression, the apical cup, with concentric rings. Throughout the length of its body many convoluted tubules occur, with unknown function. The cytoplasm contains several mitochondria and a single nucleus.
The sporozoites within half an hour of their entry into the blood stream of man, takes refuge in the liver parenchyma cells. They remain within the parenchyma cells for about seven days and during this period, each sporozoite develops into an oval Schizont of about 40 µm long (Greek: schizo, to split; onto, a being), which carries on multiple fission or schizogony.
This phase of multiplication within the parenchyma cells is called Pre-erythrocytic cycle. Each schizont produces about 12,000 merozoites (Greek: meros, a part; zoon, animal). These pre- erythrocytic merozoites are set free by the rupture of the schizont.
The newly produced merozoites travel to liver sinusoids from where they either invade fresh parenchyma cells or red blood corpuscles to initiate the erythrocytic stages of development. Each merozoite measures about 1.5 to 1.75 µm in length and 0.5 µm in breadth. It consists of an oval mass of cytoplasm with a central chromatin dot.
B. Erythrocytic Cycle:
The merozoites on entering the red blood corpuscles assume a rounded disk-like shape and soon develop into trophozoites. The young trophozoites grow at the expense of the haemoglobin of the red blood corpuscles.
It absorbs haemoglobin both by general body surface and pseudopodia. Soon after the entry of the merozoite into its body, the RBC develops a non-contractile vacuole and the nucleus is pushed to one side. The shape of the trophozoite at this stage resembles a ring and is called signet-ring stage.
It takes about 36 to 40 hours for the trophozoite to be fully grown and it occupies the whole of the RBC. At this time it multiplies by schizogony. When the schizont bursts a number of erythrocytic merozoites are set free. These merozoites enter fresh red blood corpuscles and the cycle is repeated.
Changes in the RBC and Pigment Production:
(i) Changes in Size:
As the trophozoite grows, the invaded RBC also enlarges and becomes almost double its normal size.
(ii) Changes in Shape:
The red blood cells become greatly distorted in shape, being rhomboidal or irregular in outline.
(iii) Colour Changes:
The infected RBC looses its colour. It gradually becomes colourless probably due to the loss of haemoglobin.
(iv) Changes in Appearance:
A characteristic dotted or stippled appearance is seen in infected RBC of Plasmodium vivax and is called Schuffner’s dots.
(v) Number of Parasites Invading Red Blood Corpuscles:
In Plasmodium vivax a single parasite invades each red blood cell. Double or multiple invasion is rarely seen.
(vi) Production of Pigment:
The parasite on utilization of haemoglobin as its food, yellowish-brown pigment granules appear in its cytoplasm after a period of about 10 hours growth. These pigments are often referred to as haemozoin (Greek: haemos, blood; zoon, animal).
C. Exo-erythrocytic Cycle:
The merozoites of the erythrocytic cycle enter fresh RBC and carry on exo-erythrocytic schizogony. As a result each schizont produces about 1,000 exo-erythrocytic merozoites which invade fresh RBC and continues their intra-corpuscular life cycle. It is repeated every 48 hours. The parasite when present in sufficient numbers, bring on a clinical attack of malaria.
All the merozoites do not invade new red blood cells, but some are destroyed by the phagocytic activity of the neutrophil granulocytes and the mononuclear cells of the reticulo-endothelial system.
A single infection with Plasmodium vivax may exist in the human body for a period of three years, after which it generally dies out. By this time all the exo- erythrocytic parasites which have persisted are also exhausted in the production of the erythrocytic phase.
D. Sexual Cycle:
After the schizogony has continued in the RBC for a certain period. Some of the merozoites instead of developing into trophozoites and schizonts, give rise to gamonts or gametocytes (Greek: gametes, husband or gamete, wife; kytos, cell) which has the power of sexual reproduction.
There are two forms of fully grown gametocytes — the female or macro-gametocyte and male or microgametocyte. The macro-gametocytes are larger in size, and contain many pigment granules. Their nucleus is found and situated marginally.
The nucleus of micro gametocyte is centrally located. In case of Plasmodium vivax the gametocytes appear in the peripheral blood from the first day of the fever. In the peripheral blood, the number of macro-gametocytes is greater than that of micro-gametocytes.
Further development of the gametes does not take place within the human body. Gametocytes do not cause any febrile reaction in the human host and are responsible only for the propagation of the species.
When a female Anopheles mosquito bites an infected man, the ingested blood fills her stomach. In the stomach, the macro-gametocyte becomes spherical and transforms into the macrogamete. The microgametocyte undergoes marked changes.
Five minutes after ingestion, it becomes spherical and five to six filamentous motile appendages emerge by a process called ex-flagellation. These appendages are not true flagella but are male individuals or microgametes. The microgametes start moving freely towards the macrogametes and ultimately one microgamete fertilizes one macrogamete. Fertilization occurs ten minutes after the ingestion of blood.
After 24 hours the fertilized macrogamete or zygote becomes elongated in shape and motile in habit. In this new state it is called the ookinete (Greek: oon, egg; kinetos, motile) and owing to the nature of its worm-like movement it is often called a travelling vermicule.
The ookinete measures 18 to 24 µm in length. It bores its way through the internal lining of the mosquito’s stomach, penetrates into the tissues and finally comes to rest just under the outer layer of the stomach wall.
The ookinete in this new site becomes rounded and encased in a covering or cyst derived partly from the stomach tissue and partly from its own Secretion. It is now termed the oocyst (Greek: kystis, bladder) or sporont and its development takes about 40 to 48 hours.
In P. vivax the oocyst measures about 6 to 12 µm in diameter, possesses a single vesicular nucleus and contains the pigment granules of the macrogamete. The pigment granules are in the form of numerous thin rods (seldom exceeds 70) arranged without any definite pattern and are light brown in colour.
The oocyst grows and increases in size inside the stomach wall. It bulges on the outer wall of the stomach towards the haemocoele and renders the stomach wall blistered. The cytoplasmic content of the oocyst becomes vacuolated. The nucleus divides into a large number of daughter nuclei and the protoplasm is collected around each of it.
Further nuclear multiplications result in the formation of enormous number of slender falciform or sickle-shaped bodies with pointed ends called sporozoites (Greek: sporos, seed). Each sporozoite measures 15 µm in length and 1 to 2 µm in breadth, with a central nucleus.
The first division of the zygote is believed to be meiotic in nature. The sporogony cycle is completed in about 11 days. The muscular wall enveloping the oocyst bursts and cluster of sporozoites are liberated in the haemocoele. The sporozoites are distributed throughout the mosquito’s body and invade all organs and tissues except ovaries. Infection of the salivary glands occurs between the tenth and twelfth day.
The sporozoites by virtue of their motility penetrate and lie inside the cells of the salivary glands. Such an infected female Anopheles mosquito transmits the infection to another susceptible person when it injects saliva during a bite. The sporozoites which do not find their way into the salivary glands, but pass into other parts of the body, ultimately perish.
The tissue phase of Plasmodium vivax:
Life Cycle of Plasmodium falciparum:
Etymology:
Latin: falx, a sickle. The species name “falciparum” was given as the parasite possesses sickle-shaped gametocytes.
Life Cycle:
The life cycle of Plasmodium falciparum may be divided into the following stages:
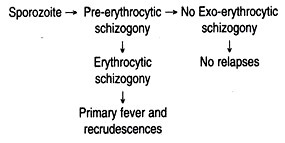
There is no exo-erythrocytic cycle in Plasmodium falciparum.
A. Pre-erythrocytic Cycle:
This refers to the development of the sporozoite during the incubation period and terminates on the first appearance of parasites in the red blood corpuscles. This cycle begins with the innoculation of the parasite as sporozoite by the bite of the infected female Anopheles mosquito into the blood stream of man.
The sporozoites exist in the blood stream from a few minutes to half an hour. The blood during this sub-inoculation period is found to be noninfectious for the first six days. The sporozoite takes refuge in the liver parenchyma cells. The first division of the sporozoite results in the formation of cryptozoites that are contained in a cryptozoic schizont. The pre-erythrocytic schizogony comprises of a single cycle and lasts for 6 days.
B. Erythrocytic Cycle — Trophozoite:
The trophozoite measures 1.25 to 1.5 µm in diameter (about one sixth the diameter of a red blood cell). The trophozoite consists of a fine and uniform cytoplasmic ring with a chromatin dot often projecting or lying beyond the ring.
A characteristic feature of this trophozoite is its tendency to attach to the margin of the host-cell with its chromatin dot. This is known as “form applique or accole”, owing to the small size and fineness of the ring. The chromatin dot may undergo early division into two.
A single red blood corpuscle may undergo multiple infection of parasite (2 to 6). This is a common feature of more than one this parasite and is not seen in any other variety. When a number of rings are present, each one is capable of developing independently in the same host-cell.
Effect on Host-cell:
While the infected red blood cells remain unaltered, the corpuscles containing the rings occasionally show a crenated appearance at its periphery. Schuffner’s dots are not seen but in their place Maurer’s dots are occasionally found. The Maurer’s dots are fewer in number, coarser, more irregular in shape than Schuffner’s dots.
P. falciparum while growing inside the red blood cells, have a tendency to adhere to one another and also to the endothelium of the capillaries of internal organs, forming clumps and thereby obstructing the flow of blood.
Schizont:
The schizogony of P. falciparum is restricted particularly inside the capillaries of the internal organs, specially in the sinuses of the spleen, liver and bone marrow. This parasites particular choice of location is the bone marrow of the ribs.
When the pigment starts appearing in the cytoplasm of the parasites, they are filtered out by the capillaries of the internal organs. By this time the ring form increases in size, measuring 4 µm in diameter.
The vacuoles gradually disappear and the parasite accrues a compact form, each containing a single chromatin material. The chromatin material divides into several masses (8 to 32 in number) and each of them accrues a small piece of cytoplasm around it. The mature schizont measures 4.5 to 5 µm in diameter.
Merozoite:
The number of merozoites varies considerably and their average number being 18 to 24. Individual merozoites are very small in size measuring 0.5 to 0.7 µm in diameter. The life cycle of schizogony is completed between 36 and 48 hours. However, the completion of each generation is often irregular.
The liberation of merozoites does not coincide with the convulsion of fever, as at any given time some parasites may be undergoing division. Thus, in case of P. falciparum infection there is always the occurrence of remittent and irregular type of temperature. As compared to other human plasmodia, the life-span of P. falciparum is much shorter. Long term relapses as seen in P. vivax, also do not occur.
C. Sexual Cycle:
After the continuation of schizogony for a certain period, some of the merozoites give rise to gamonts or gametocytes, which perform a sexual method of reproduction.
The sexual forms of P. falciparum are characterized by their peculiar shape and are also easily recognised from the growing schizonts even at an early stage. The sexual forms look more like sausages or beans with rounded ends and are generally known as “crescents” or “half-moon bodies”.
With the maturation of gametocyte, the red blood cell gets gradually used up and only its skin remains, which encloses the parasite in the form of a sheath. The mature gametocyte is about one and a half times larger than the RBC in which it is present.
In primary infection, after 7 to 13 days of fever, the gametocytes appear in the peripheral blood. The number of gametocytes is always greater in the peripheral blood (50,000 to 1,50,000 per ml. of blood) as compared to other species of plasmodia. The number of females is always -more than that of the males (about 3 to 1 or even as much as 6 to 1).
The macro-gametocytes are generally longer and narrower, with their ends being sharply rounded or even pointed. They are 10 to 12 µm in length and stain deep blue with Romanowsky’s stains. The chromatin material is in a small compact mass and the pigment granules surround it.
The microgametocytes on the other hand, are shorter and broader, with their ends being bluntly rounded. They are 8 to 10 µm in length and stain reddish or pinkish-blue with Romanowsky’s stains. The chromatin material and pigment granules are irregularly distributed.
P. falciparum infections exhibit successive waves of trophozoites and gametocytes (considered as one unit). In longer attacks there may be several such units. Once the mature gametocytes have appeared in the peripheral blood, they remain for a long period and their life span has been found to be 30 to 60 days.
Subsequent development of the gametocytes occurs only when they are taken up by the female Anopheles mosquito and further development takes place in it. The gametocytes ingested by the mosquito are liberated within the new host’s gut.
After further development, the male gametocyte (microgametocyte), fuses with the female gametocyte (macro-gametocyte) to form a zygote. The zygote penetrates the stomach wall of mosquito and gives rise to a large number of sporozoites. This stage migrates into the salivary glands of the mosquito and is introduced into the next human host by its bite.
The tissue phase of P. falciparum:
Malaria vectors in W. Bengal:
The malaria causing vectors in W. Bengal comprise of the following species of Anopheles:
i. In the plains — A. philippinensis
ii. In the sub-mountain areas — A. minimus
iii. In the deltaic areas — A. sundaicus
iv. In the city of Kolkata — A. stephensi
A. culicifacies is widespread in W. Bengal, but they are not important as a malaria- carrier.