The below mentioned article provides a study note on the Placentation in Human.
Implantation of Placenta in Human:
When the developing human egg following fertilization, reaches the uterus it is still surrounded by the zona pellucida and the corona radiata. The blastocyst remains free and floating within the uterus for about four days.
During this time it maintains itself through the exchange of oxygen, fluid, ions and nutrients across the zona pellucida. By the 7th day after fertilization, the zona pellucida starts breaking down (this is often called the “hatching of the blastocyst”) and the embryo is now ready to undergo implantation in the endometrium.
ADVERTISEMENTS:
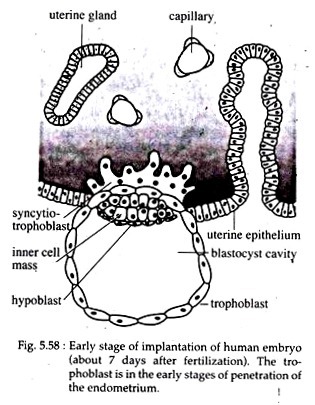
The first step in implantation is attachment, where the developing embryonic trophoblast adheres itself to the hormonally prepared uterine epithelium. Attachment of the trophoblast occurs at the end containing the inner cell mass (Fig., 5.58).
In case, the uterine epithelium is not hormonally prepared then it will not be able to participate in the attachment. On the other hand, if the uterine epithelium is scraped off, the embryo can implant onto the endometrial stroma at any time.
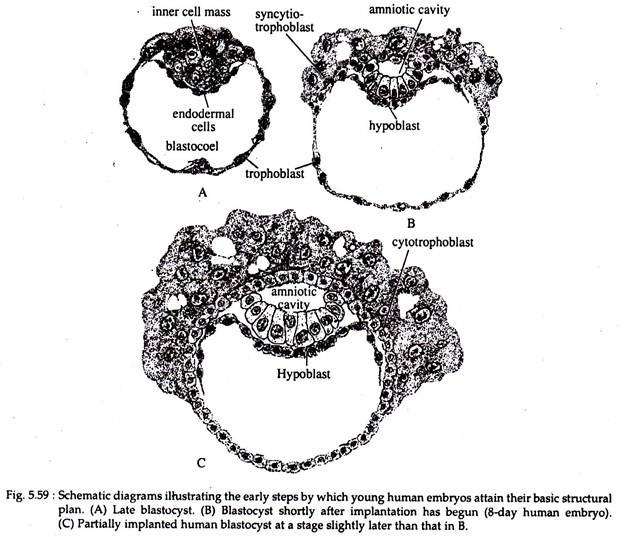
In the next step of implantation, the uterine epithelium becomes erroded in the area of immediate contact with the blastocyst and the trophoblast begins to invade the maternal tissue. The epithelial cells of the trophoblast layer of the blastocyst increases in number. The trophoblast tissue thus enlarges greatly at the contact area (Fig. 5.59).
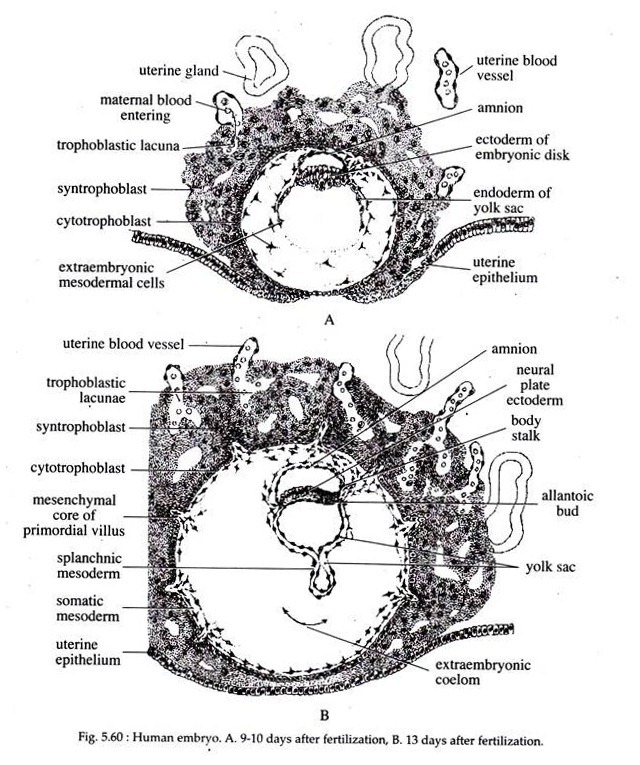
At this stage a change occurs in the trophoblast cells. Its external cells fuse together to form a syncytium and is called syncytiotrophoblast or syntrophoblast. The inner trophoblast cells, on the other hand, remain cellular and are called cytotrophoblast (Fig. 5.60A). The syntrophoblast acts as the invading tissue.
By the 11th or 12th day, the blastocyst becomes completely embedded within the endometrium (Fig. 5.60) and the uterine epithelium grows back over the embryo. Soon thereafter, irregular spaces called the trophoblastic lacunae appear within the expanding syntrophoblast and these lacunae get filled with maternal blood (Fig. 5.60). This marks the beginning of the haemochorial placenta.
Extra Embryonic Membranes of Human Embryo:
ADVERTISEMENTS:
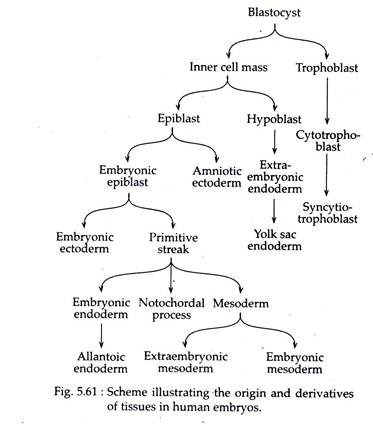
It was believed previously that in human the extra embryonic tissues arise from the trophoblast. However, recent experiments have shown that the original trophoblast gives rise only to the cytotrophoblast and syntrophoblast. The remainder of the extra embryonic tissues come from the inner cell mass (Fig. 5.61).
Formation of Chorionic Villi:
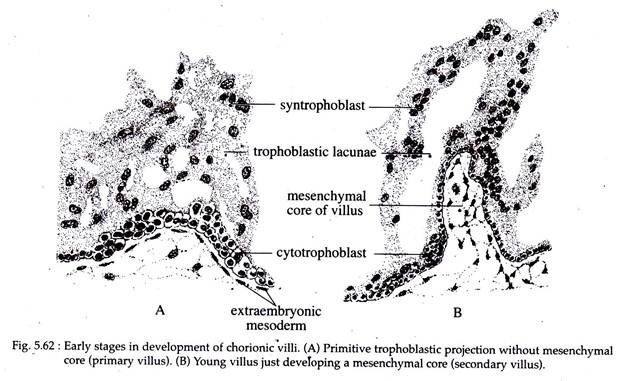
By the end of the 2nd week of gestation period, the trophoblast of the human embryo begins to be molded into masses and starts forming villi. The young villi at first consist entirely of epithelium, without any connective tissue and is thus referred to as the primary villi (Fig. 5.62A).
This phase of the villi where it lacks a mesenchymal core is very short-lived. In the early 3rd week after fertilization, the mesoderm pushes into the primitive villi and forms a framework of delicate connective tissue covered by the epithelial layer.
These villi are called secondary villi (Fig. 5.62B). Soon, blood vessels appear in the connective tissue core period, the trophoblast of the human embryo begins to be molded into masses and starts forming villi.
The young villi at first consist entirely of epithelium, without any connective tissue and is thus referred to as the primary villi (Fig. 5.62A). This phase of the villi where it lacks a mesenchymal core is very short-lived. In the early 3rd week after fertilization, the mesoderm pushes into the primitive villi and forms a framework of delicate connective tissue covered by the epithelial layer.
These villi are called secondary villi (Fig. 5.62B). Soon, blood vessels appear in the connective tissue core of the villus and extend into the newly formed branches. Such villi with a vascular connective tissue core are known as tertiary villi and this condition is reached by the end of third week.
ADVERTISEMENTS:
Meanwhile, some of the endometrial tissues at the invading point of the chorionic vesicle, breaks down (including blood vessels) to form liquefied areas called the embryotroph.
Formation of Placenta:
Striking changes take place in the endometrium particularly at the place of implantation. Here, the stromal cells of the uterus become filled with glycogen and lipid droplets and are called decidual cells. These cells at the termination of pregnancy are shed and then rebuilt. The term decidua (meaning to shed) has come from the phenomena of shedding and replacement.
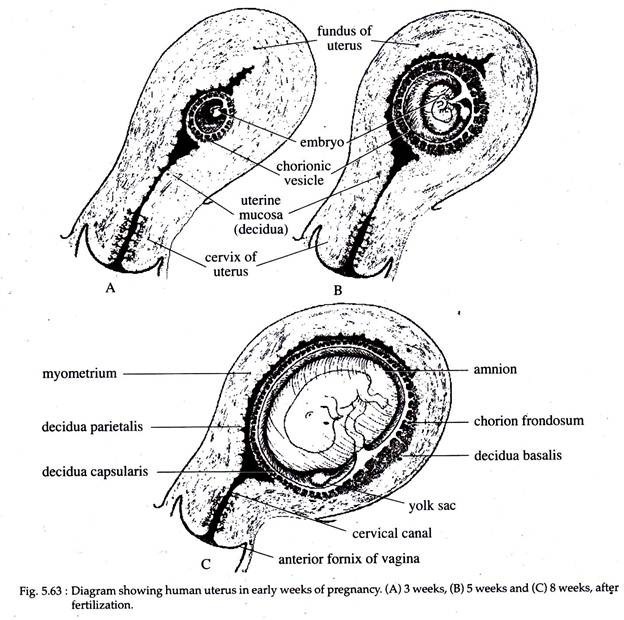
The human embryo promptly burrows into the endometrium. As its developing chorionic vesicle grows within the endometrium, the uterine mucosa expands over the growing vesicle, forming a layer known as the decidua capsularis (Fig. 5.63).
The portion of the endometrial lining of the uterus not concerned with the enclosure of the chorionic vesicle is called the decidua vera or decidua parietalis. The portion of the endometrium lying immediately next to the enlarging villi of the chorionic
.
The chorionic villi at first are developed over the entire chorionic vesicle (Fig. 5.63A and B). But, as development proceeds the villi in the decidua capsularis are reabsorbed gradually and this part has no direct role in the nutrition of the embryo. This part of the chorion that has lost its villi becomes smooth and is called the chorion laeve.
Only those villi present in relation to the decidua basalis remain. They enlarge and become the main villi for physiological exchange between the embryo and the endometrium. This portion of the chorionic vesicle in the decidua basalis is known as the chorion frondosum (Fig. 5.63C).
The interlocked chorion frondosum of the foetus and decidua basalis of the mother form the placenta. The placenta is thus a dual structure composed of the decidua basalis or maternal placenta and the chorion frondosum or foetal placenta.
The early chorionic villi at about the 4th week of pregnancy is composed of four parts:
(1) Blood capillaries present within it,
(2) The mesenchymal cells of the mesodermal core,
(3) Cytotrophoblast,
(4) Syntrophoblast.
However, as development proceeds, the mesenchymal core with its blood capillaries increases in size and the cytotrophoblast decreases in quantity. At about the 4th month, the cytotrophoblast is represented by a few scattered cells.
The placental villi are grouped together into cotyledons and in-between them are the placental septa which incompletely separates the various cotyledons from one another. Surrounding the villi within each cotyledon is a pool of maternal blood. In it is bathed the syntrophoblast of the villi. Thus, a haemochorial relationship has been established.